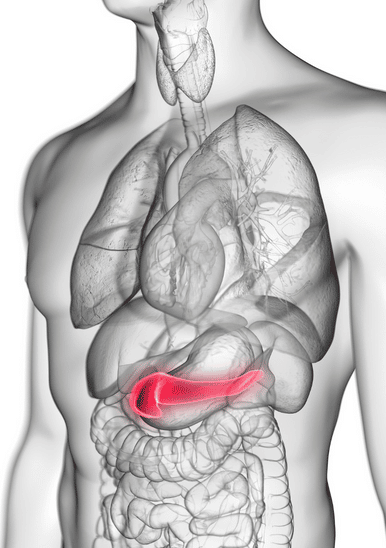
The pancreas is an essential gland that produces enzymes that aid in digestion and regulate the way your body processes sugar. Inflammation of the pancreas is known as pancreatitis.
This inflammation can occur as acute pancreatitis, which is quite mild and can last for a few days. Chronic pancreatitis is much more severe and may occur over many years.
The chances of suffering from pancreatitis may arise due to damage caused to the pancreas by certain health conditions.
In addition, certain lifestyle choices may also increase the risk of developing pancreatitis, such as:
Smoking
Overconsumption of alcohol
Unhealthy eating habits that may cause obesity
Family history of pancreatitis
Symptoms of pancreatitis
Symptoms may vary depending on whether you’re suffering from acute or chronic pancreatitis.
If you’re experiencing any of the following symptoms, you might want to visit your healthcare provider immediately for a prognosis.

You may have acute pancreatitis if you display the following symptoms:
- Upper abdominal pain
- Tenderness of the abdomen
- Fever
- Nausea and vomiting
- Rapid pulse

You may have chronic pancreatitis if you display the following symptoms:
- Upper abdominal pain
- Pain in the abdomen after eating
- Unintentional weight loss
- Oily, smelly stools
Screening and diagnosing pancreatitis
Seeking immediate medical attention can allow your healthcare provider to prescribe relevant measures of treatment to ease your discomfort.
Your doctor may subject you to a series of tests to obtain an accurate diagnosis before providing any treatment.
You might be recommended to follow through with the following procedures:
Blood tests may be done to look for elevated levels of pancreatic enzymes, white blood cells, liver enzymes, and good functioning of the kidneys
Endoscopic ultrasounds may be done to detect any signs of inflammation and blockages in the bile duct and pancreatic duct
Magnetic Resonance Imaging (MRI) scans may be performed to detect any abnormalities in the pancreas, gallbladder, and ducts
Abdominal ultrasounds may be requested by your doctor to detect or eliminate the possibility of gallstones and pancreatic inflammation
Stool tests may be carried out to help determine if you have acute or chronic pancreatitis as they can suggest how well your digestive system is absorbing nutrients.

Complications of pancreatitis
Once your physician diagnoses you with either acute or chronic pancreatitis, you’ll be prescribed all the necessary methods of treatment.
If you fail to go ahead with the prescribed treatments or don’t get a timely diagnosis, you’ll likely start to experience serious pancreatitis long-term effects and complications, including:
Breathing difficulties
Acute pancreatitis may cause chemical changes in your body that may affect the functioning of your lungs, causing your blood oxygen levels to drop dangerously low.

Failing kidneys
Acute pancreatitis may also cause your kidneys to fail. Severe kidney failure can be treated with dialysis.

Developing an infection
Your pancreas is more vulnerable to bacteria if you’re suffering from acute pancreatitis. The chances of developing an infection are high and surgery may be required to remove the infection.
Risking malnutrition
Malnutrition may arise due to acute and chronic pancreatitis because there are fewer enzymes to break down and process nutrients.

Causing diabetes
Chronic pancreatitis can cause damage to the insulin-producing cells in your pancreas which may fail to efficiently process sugars, leading to high levels of blood sugar.
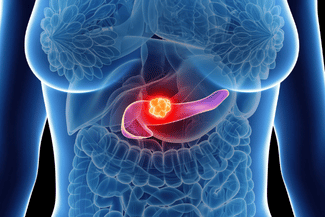
Increasing the risk of pancreatic cancer
If unattended for a long period, the inflammation in your pancreas caused by chronic pancreatitis can increase the risk of developing pancreatic cancer.
Managing pancreatitis long-term effects
Your physician might be able to provide you with management measures to reduce your levels of discomfort and prevent the pancreatitis long-term effects from escalating further.
Methods of management may include:
Eating on time: As soon as you’re able to eat normal quantities of food, start consuming bland foods and clear liquids; this can help heal the pancreas and reduce inflammation
Intravenous fluids (IV): May be administered to provide proper hydration; your body might become dehydrated as most fluids are being used up to repair the pancreas
Pain medications: May be prescribed by your physician as acute and chronic pancreatitis may cause you to be in a lot of pain
Enzymes to improve digestion: Digestive enzymes, for example, may be prescribed to help your body break down and process the nutrients you consume
Changes to your diet: Your healthcare provider might recommend you to a dietician who can create a low-fat diet plan that’s high in nutrients
A gastrointestinal specialist can help you in managing pancreatitis long-term effects
Sydney-based gastroenterologist and hepatologist Dr Suhirdan Vivekanandarajah specialises in providing expert medical care for gastrointestinal-related illnesses.
Schedule a consultation today and find out how you can improve your digestive health.
