What is ulcerative colitis?
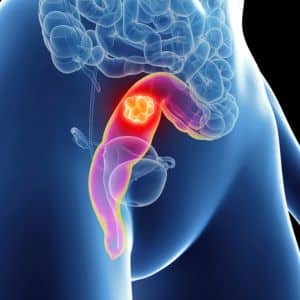
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that affects the colon and rectum. Ulcerative colitis shows swelling and ulcers along the lining of the large intestine, which can lead to various signs like abdominal pain, diarrhoea with blood in it, rectal bleeding, and urgency for bowel movements.
The symptoms may have different levels of severity and effects, often causing disturbances in everyday living and general health. The reason for ulcerative colitis remains unknown, but it’s thought to be triggered by a mix of genetic, environmental, and immune system factors.
Remember, learning about the possible treatments for ulcerative colitis is important so people can handle it effectively and improve their quality of life.
What is the impact of UC on daily life and health?
Ulcerative colitis might affect your everyday life and the general health of people diagnosed with this medical condition. The influence differs for each person based on how severe their disease is and the effectiveness of ulcerative colitis treatment in Australia.

Physical health
Ulcerative colitis significantly impacts physical health. Symptoms such as often having stomach pain, cramps, and continuous diarrhoea can be tiring and debilitating. Bleeding from the rectum or feeling a constant need to use the bathroom can be highly distressing for patients. Long-lasting inflammation and high frequency of bowel movements are common triggers for insufficient absorption of nutrients, which can result in vitamin and mineral deficits, and may result in medical conditions like anaemia and a considerable drop in body weight. Furthermore, constant inflammation combined with the body’s immune system response can cause significant fatigue, which makes it difficult to carry out daily activities and lowers overall energy levels.

Mental and emotional health
Ulcerative colitis is unpredictable. People with ulcerative colitis often worry about whether there are enough bathrooms and they might have an accident that could make them feel embarrassed, causing extra anxiety in public or social occasions. Living with a long-lasting sickness can also make someone feel alone, sad and downcast. This is especially true when there have been significant changes to their lifestyle and social activities. Useful methods for handling the emotional effects of ulcerative colitis include developing good coping skills and having a solid support network. Therapy, groups that give support, and other resources can assist patients with the mental and emotional problems that come up when living with ulcerative colitis.

Social and professional life
Ulcerative colitis hinders and causes problems in work and school pursuits. People with ulcerative colitis might have symptoms that can disrupt attendance and performance, necessitating time off for medical appointments, treatments, and severe flare-ups if and when they occur. Additionally, socialising and participating in activities could be restricted by the requirement to stay near a bathroom as well as the fear of unexpected symptoms appearing. This might cause public isolation anxiety impacting their personal connections and social involvement. For ulcerative colitis patients, making plans for trips and journeys could be extra stressful because they have to think about toilet access and how travel might exacerbate their symptoms.

Quality of life
Ulcerative colitis patients undergo a significant change in their quality of life, which can disturb daily routines and may necessitate important modifications to lifestyle, like strict timing for medications, limits on what they eat or regular visits with gastrointestinal specialists. There are also health complications that happen for a long time with ulcerative colitis, like a higher possibility of colon cancer and weak bones, also known as osteoporosis or liver disease. Regular monitoring and preventive care are essential to manage these risks effectively. Dealing with a long-term and chronic condition like ulcerative colitis can be a financial burden because of the constant need for medication, treatments, and visits to the doctor.
Recognising the many sides of ulcerative colitis emphasises the need for good handling and complete care. A total strategy that deals with physical signs as well as mental, emotional, and social difficulties related to the medical condition, could significantly improve the quality of life for people diagnosed.
What are the types of surgery and ulcerative colitis treatment in Australia?

Colectomy
Colectomy is a surgical procedure involving the removal of a portion or the entirety of the colon. There are two primary types of colectomy: total colectomy and partial colectomy.
Proctocolectomy
Proctocolectomy is a surgical procedure involving the removal of both the colon and the rectum. The two main types of proctocolectomy are total proctocolectomy and subtotal proctocolectomy.

Ileal Pouch-Anal Anastomosis (IPAA or J-Pouch)
This is a complex surgical procedure that creates a reservoir within the body for stool storage and elimination in individuals who have undergone removal of the colon and rectum.

Ileostomy
A surgical procedure that involves creating an opening in the abdominal wall through which a portion of the small intestine is brought to the surface when the colon and rectum are removed.
What are the considerations and implications of ulcerative colitis treatment in Australia?
Every kind of surgery for ulcerative colitis has its advantages and points to think about. The decision on which surgery to choose is based on factors such as disease severity, patient preferences, and the expertise of the surgical team.
Reversibility
Certain surgeries such as subtotal colectomy and IPAA can be reversed but total proctocolectomy with a permanent ileostomy is irreversible.
Functional results
IPAA surgery tries to maintain continence and bowel function, while an ileostomy might need considerable adjustments.
Complications
Surgeries come with risks, such as infection, bleeding, and obstruction in the bowel. Patients should discuss these possible complications with your healthcare team.
Quality of life
Surgery has the potential to considerably enhance the quality of life for numerous ulcerative colitis patients by relieving symptoms and decreasing the chances of complications such as colon cancer.
Continuing care
In the future, patients will need to be observed and possibly adjust to their surgical procedure over time. They might also require support in adapting to life with an ostomy if they have one.
What are biologics?
Biologics are a group of medications for dealing with different medical conditions, which can also treat health problems such as ulcerative colitis. Unlike traditional medications, which are synthesised chemically, biologics are derived from living organisms or their components. They usually are large complex molecules made of proteins, antibodies, and nucleic acids which are engineered to target specific parts of the immune system.

What is the availability of biologics in Australia?

In Australia, you can get biologics for treating ulcerative colitis through various channels, including public and private healthcare systems. Biologics can be accessed via the Pharmaceutical Benefits Scheme (PBS) for qualified patients. This scheme offers reduced-cost access to specific medicines.
The availability and access to certain biologics can change depending on various elements like the personal features of a patient, how serious their illness is, and what particular healthcare provider they use. Patients should talk with their gastrointestinal specialist about possible biologic treatments suitable for their condition.
What are the tips for patients to manage ulcerative colitis effectively with available resources?
Through the use of medications, surgery, and changes in diet, along with a multidisciplinary method, patients can handle ulcerative colitis; this helps them keep symptoms down and enhance their quality of life.
Educate yourself
Obtain knowledge from dependable sources, materials for patient education, and groups giving support to learn about ulcerative colitis, methods of treatment, and ways of managing it.
Communication
Always speak honestly and openly with healthcare providers, voice worries or concerns, ask for explanations when needed, and take part actively in choices about treatment.
Compliance with treatment plans
Keep to medication schedules, visit the doctor on time, follow what they suggest, and stick to dietary advice for the best results in treatment.
Symptom monitoring
Use diaries or mobile applications to record ulcerative colitis symptoms, triggers, and possible side effects of medications. This can help gastrointestinal specialists understand disease activity and adjust treatment as needed.
Seek support
Rely on family, friends, and support systems such as online communities or local groups to provide emotional assistance, practical suggestions, and similar encounters.
Utilise resources
Use available resources like educational materials, patient advocacy organisations, and healthcare navigators to get information, financial help, or support for services.
Empowering patients with knowledge, support, and resources is key to achieving optimal outcomes in ulcerative colitis management.
FAQs

The exact cause is unknown, but it is believed to be due to an abnormal immune response, genetic factors, and environmental triggers. The immune system mistakenly attacks the cells in the digestive tract.
There is currently no cure for UC, but many patients achieve long-term remission with proper treatment and lifestyle adjustments under the recommendations of a gastrointestinal specialist.
Ulcerative colitis can be considered a disability in Australia if it significantly impacts an individual's ability to perform daily activities or work tasks. Eligibility for disability benefits or accommodations would depend on the severity of the condition and its impact on the individual’s functioning.
Consult a gastrointestinal specialist for ulcerative colitis treatment in Australia
Take control of your ulcerative colitis management today. Schedule a consultation with a trusted gastrointestinal specialist in Australia and embark on your journey towards better health. Don't let your gastrointestinal conditions hold you back—book your appointment now.
