What are the causes of rectal bleeding?
Rectal bleeding can have various causes, ranging from benign conditions such as haemorrhoids and anal fissures to more serious conditions such as colorectal cancer and inflammatory bowel disease (IBD).
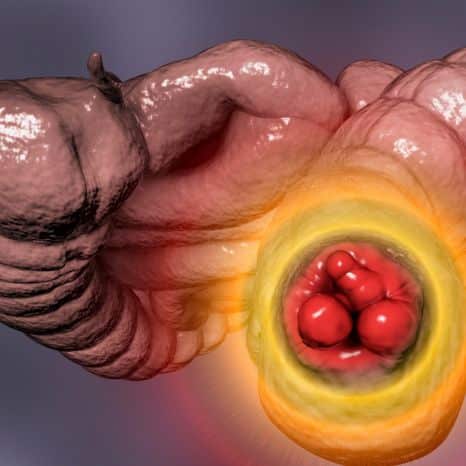
Haemorrhoids
Haemorrhoids are swollen blood vessels in the rectum or anus. Straining during bowel movements, chronic constipation, and prolonged sitting can contribute to the development of haemorrhoids.

Anal fissures
Anal fissures are small tears or cracks in the lining of the anus, often caused by passing hard stools or straining during bowel movements. These fissures can result in pain, itching, and bleeding.

Inflammatory bowel disease (IBD)
Chronic inflammation of the GI tract could mean Crohn’s disease or ulcerative colitis, and can be accompanied by diarrhoea, abdominal pain, rectal bleeding, and weight loss.
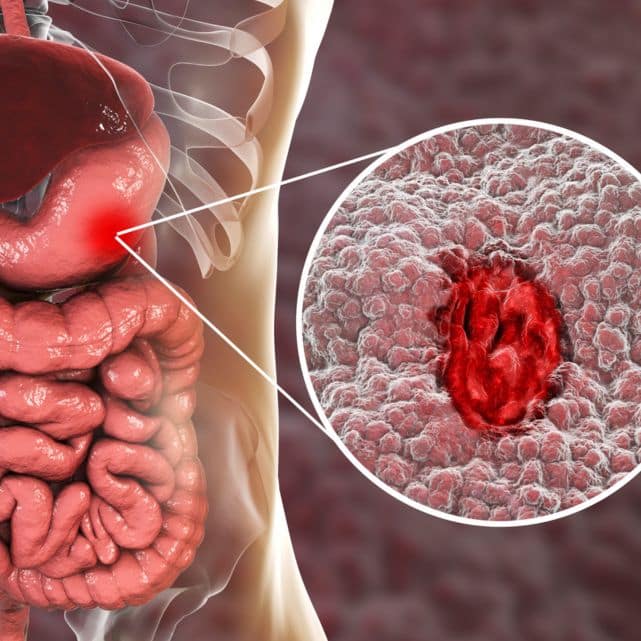
Colorectal cancer
Abnormal cells in the colon or rectum grow, forming tumours. Rectal bleeding is a symptom of colorectal cancer, in its early stages, with changes in bowel habits, abdominal pain, and weight loss.

Anal cancer
Anal cancer is a rare type of cancer that develops in the tissues of the anus. Rectal bleeding, pain or pressure in the anal area, and changes in bowel habits are common symptoms of anal cancer.

Diverticulosis
Diverticulosis refers to the presence of small pouches in the walls of the colon. When these pouches become inflamed or infected, it can lead to rectal bleeding, abdominal pain, and changes in bowel habits.
It is important for individuals experiencing rectal bleeding to seek medical evaluation and diagnosis to determine the underlying cause and appropriate rectal bleeding treatment.
How can certain dietary factors contribute to or alleviate rectal bleeding?
Understanding how dietary choices can contribute to or alleviate rectal bleeding is crucial for managing the condition effectively.
Fibre intake
Fibre intake is essential for maintaining digestive health and preventing constipation, which is a common cause of rectal bleeding. Fibre adds bulk to stools, making them softer and easier to pass, thus reducing the need for straining. This, in turn, helps to prevent irritation and trauma to the rectal area. Foods that are rich in fibre include fruits, vegetables, whole grains, legumes, nuts, and seeds. Incorporating these foods into the diet can promote regularity and reduce risks of rectal bleeding.
Hydration
Staying hydrated is important for passing bowel movements and effective digestion. Drinking an adequate amount of water is important for softening stools and preventing tightness in stools from constipation. Dehydration can lead to hard, dry stools that are difficult to pass, increasing the likelihood of straining and rectal bleeding. Therefore, staying well-hydrated by consuming plenty of water and other hydrating fluids can help maintain bowel regularity and minimise the risk of bleeding.
Avoiding constipation-causing foods
The intake of certain foods can contribute to constipation and exacerbate rectal bleeding. Processed foods, refined grains, and low-fibre foods can slow down digestion and lead to hardened stools and constipation, making bowel movements difficult and increasing the risk of straining. By limiting the consumption of these constipation-causing foods and prioritising fibre-rich alternatives, individuals can promote smoother bowel movements and reduce the likelihood of rectal bleeding.
Probiotics and gut health
Probiotics, found in fermented foods such as yoghourt, kefir, sauerkraut, and kimchi, can help to support gut health by promoting the growth of beneficial bacteria in the digestive tract. A healthy balance of gut flora is essential for optimal digestion and immune function, which can help to reduce inflammation and improve overall gastrointestinal health. Incorporating probiotic-rich foods into the diet may therefore have a beneficial effect on conditions associated with rectal bleeding.
Dietary factors play a significant role in contributing to or alleviating rectal bleeding. By focusing on a diet rich in fibre, staying hydrated, avoiding irritants, and promoting gut health, individuals can effectively manage their symptoms and reduce the risk of bleeding episodes.
Consulting a healthcare professional for personalised dietary recommendations and guidance based on individual health needs and underlying conditions.
Consult a gastro-specialist about getting rectal bleeding treatment
Emphasising the importance of consulting a healthcare professional before making significant changes to diet or lifestyle is crucial for ensuring safe and effective rectal bleeding treatment. Seeking medical guidance allows for personalised advice tailored to individual health needs, medical history, and underlying conditions. Healthcare professionals can assess risk factors, conduct a thorough evaluation to determine underlying causes, and develop appropriate treatment plans.
Dr. Suhirdan Vivekanandarajah is a distinguished gastrointestinal specialist located in Sydney, Australia. With a wealth of experience and specialised training in gastroenterology, Dr. Vivekanandarajah is renowned for delivering exceptional care and expertise across a broad range of gastrointestinal issues.
Medical specialists can help identify potential risks associated with dietary or lifestyle changes and provide guidance on minimising them. Regular monitoring and follow-up appointments enable ongoing assessment of gastrointestinal symptoms, treatment goals, and health status, ensuring appropriate care and support over time.
Dr. Vivekanandarajah’s expertise extends to the diagnosis, treatment, and management of various gastrointestinal conditions, ensuring his patients receive comprehensive and personalised care tailored to their unique needs.

FAQs

The fastest way to heal rectal bleeding depends on the cause. If it’s due to a minor issue like haemorrhoids, it might heal on its own with time and self-care measures like keeping the area clean, using over-the-counter haemorrhoid creams, and avoiding constipation. However, if it’s due to a more serious condition like inflammatory bowel disease or colorectal cancer, you should seek medical attention promptly for proper diagnosis and treatment.
Profuse rectal bleeding can be a medical emergency, and you should seek immediate medical attention by calling emergency services or going to the nearest emergency room. While waiting for medical help, you can lie down with your legs elevated and apply pressure to the bleeding area using a clean cloth or gauze. Avoid taking any medications without medical advice as they may worsen the rectal bleeding.
The best medicine for rectal bleeding depends on the underlying cause. For haemorrhoids, over-the-counter creams containing hydrocortisone or witch hazel may help reduce inflammation and bleeding. However, if the bleeding is due to a more serious condition like inflammatory bowel disease or colorectal cancer, prescription medications and other treatments may be necessary. Consulting a gastrointestinal professional for diagnosis and treatment recommendations is crucial.
